
Find hidden savings on your medical bills
Help protect against medical fraud and overbilling
More than half of medical bills contain errors,1 which can be confusing and costly. But you don’t have to navigate the healthcare system alone. HealthLock is on your side.
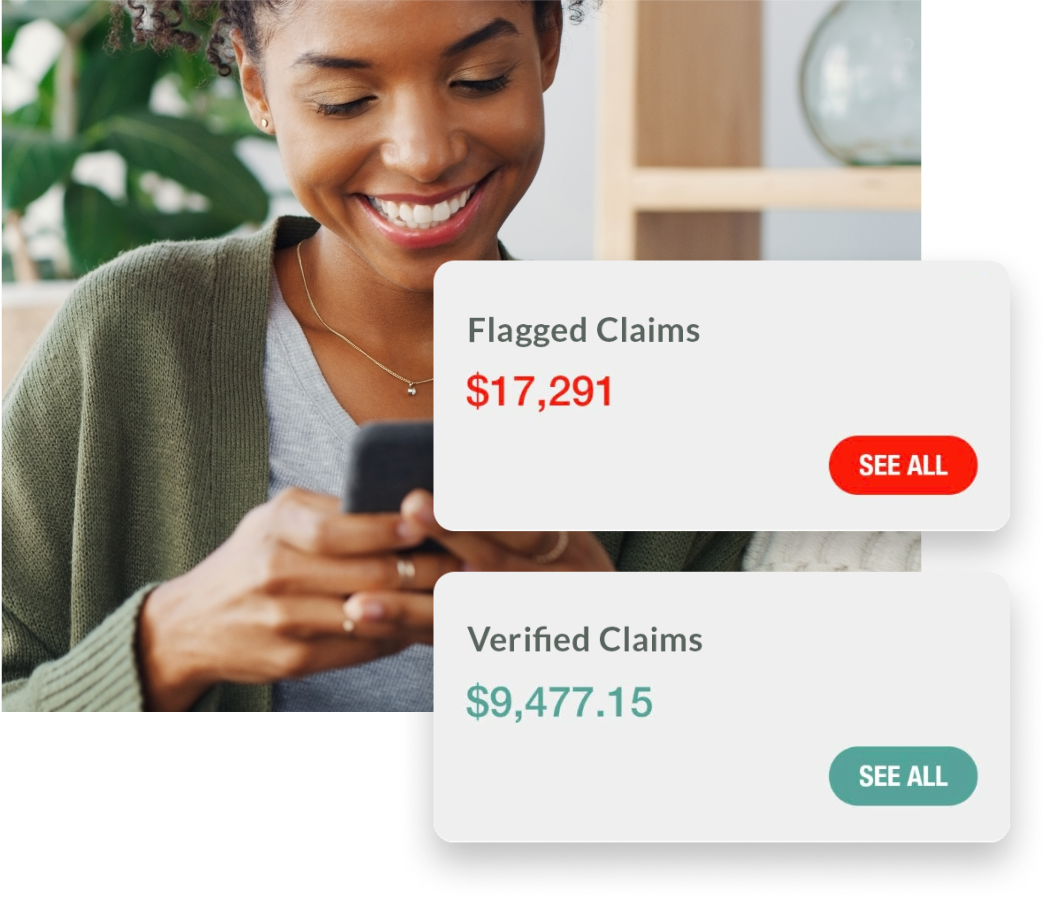
Our healthcare technology securely syncs with your insurance companies and reviews the incoming claims, flagging any potential medical fraud, errors or overbilling.
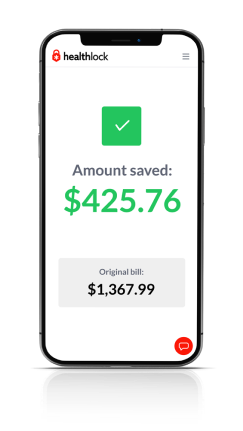
If you’ve been overcharged by a provider, you can request that we negotiate on your behalf to help get your money back.§ To date, we’ve helped our members save over $130 million.
Are you paying too much? We can help you find potential savings.
HealthLock automatically reviews medical claims for overcharges and helps get your money back.§
$325
billion
is lost to medical overbilling and fraud2
50%
over
of medical bills contain errors1

If you experience medical fraud, we’ll help fix it.**
We work 24/7 to monitor your providers for HIPAA violations and breaches of your private medical information. If your information is exposed in a breach, we’ll help restore your privacy.
59
million+
healthcare records breached in 20223
50x more
Your medical data is
valuable than your credit card on the black market4
You’re not alone. We’re here to fight on your behalf.
If you’ve been overcharged by a provider, you can request that we negotiate on your behalf.§ To date, we’ve helped our members save over $130 million.
56%
of Americans feel lost trying to understand health insurance5
66%
of bankruptcies are tied to medical issues.6
HealthLock plans

SILVER
Flags potential errors and overcharges
$9.99/mo
$0/mo
GOLD
Provides access to expert medical bill negotiations
$19.99/mo
$14.99/mo
PLATINUM
Offers financial and cyber protection
$29.99/mo
$24.99/mo
Privacy
We work around the clock to monitor your providers for HIPAA violations and breaches of your private medical information. When we detect a breach at one of your providers, we’ll alert you.
If you don’t recognize a doctor or your bill doesn’t match, just let us know. We’ll investigate to uncover whether it’s an error or a misuse of your information. If it’s fraud, our team will help fix the problem.
The only score of its kind, we calculate your privacy exposure based on several risk factors. As the score changes, we alert you via your dashboard so you can take control of your medical privacy.
We alert you by email or text whenever we detect new claims, a breach, or a potential threat. Our comprehensive alerts provide expanded notifications for our enhanced plans to help you stop medical and financial identity theft early.
Control
See all your medical claims at a glance. We bring all your insurance-submitted doctor and medical service claims into a single location for easy review and verification.
Using our powerful HealthLock DeepAudit Technology, we automatically audit incoming claims and flag potential upcoding and overcharges so you can get your money back.
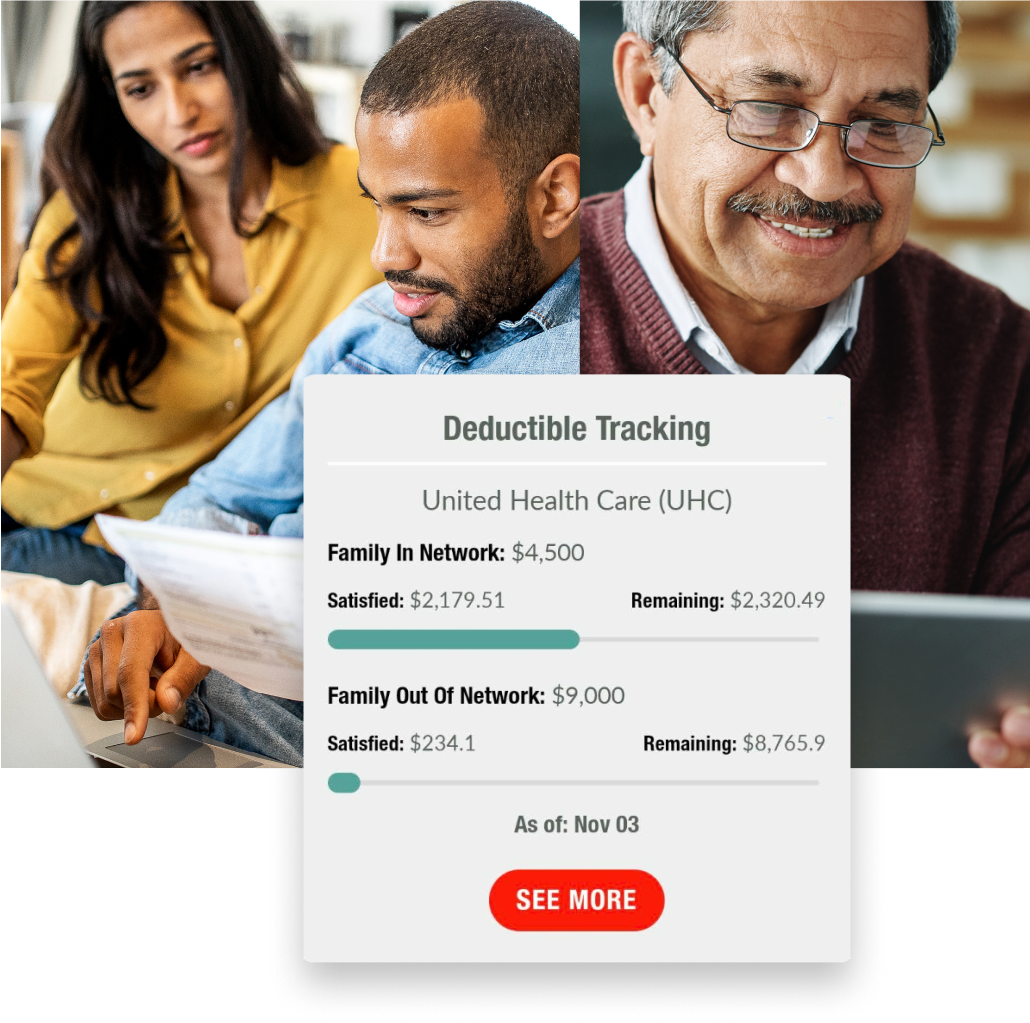
Take back control of your healthcare with our centralized, easy-to-understand dashboard. View your claims, deductibles, doctors, and more on your desktop or mobile phone. Securely upload your insurance cards, invoices, and receipts for easy access anytime.
Have a question? Our friendly team of knowledgeable experts is available via email or chat to provide advice and answer your questions about alerts, your dashboard, and your membership.
Savings
Upon joining, we’ll analyze up to two years of your previous medical claims and flag potential overcharges using our HealthLock DeepAudit technology. While in most cases these claims are past the 90-day window for negotiation, the analysis helps you identify the potential for future overbilling issues.
For select flagged bills that are less than 90 days old, you can elect to have us work on your behalf to reclaim money from overbilled and overpaid bills.
Track what medical expenses you’ve paid out-of-pocket already and know how much you have left to meet your annual deductibles.
If you’ve been overcharged by a provider, you can request that we negotiate on your behalf to help get your money back. To date, we’ve helped our members save over $130 million.
When we negotiate on your behalf, we’ll assign you to a Personal Reimbursement Specialist. While our team is busy getting your money back, they’ll be your point of contact.
How HealthLock works
Our powerful HealthLock DeepAudit technology and team of ever-vigilant professionals work around the clock to review your medical claims and flag any potential issues like overbilling or fraud.

Sync
Connect your insurance company to HealthLock. We’ll organize your claims, doctors and more in a single secure dashboard.

Monitor
We review your claims for errors while we monitor for breaches, new providers and privacy intrusions.

Alert
Anytime we detect potential overbilling, fraud or suspicious activity, we flag it and notify you immediately.

Negotiate
Optionally, you can request HealthLock investigate and negotiate overcharges to get your money back.§

Protect
We work proactively to put your doctors on watch and monitor for breaches 24/7. We always have your back.
"HealthLock negotiated on my behalf. And the insurance paid the whole thing."
"HealthLock manages my medical claims, negotiates with my insurance carriers and providers, and has saved me nearly $100,000 in medical costs."
"I love that HealthLock organizes all of my claims in one place and that they review each one."
** Remediation includes guidance throughout the recovery process, assistance in restoring accuracy to credit reports and medical records, help reporting errors to health care providers, and assistance finding new doctors. HealthLock will spend up to $1 million to cover internal expenses related to remediation. This is not an insurance product. HealthLock does not reimburse for member losses or personal expenditures. Covered expenses are provided at the sole discretion of HealthLock.
† Historical Claim Analysis and 90-Day Retro Audit and Recovery are provided once per member lifetime only during initial enrollment.
§ Negotiation and recovery services require 20% shared savings of reclaimed money or bill reduction, charged to the payment option on file upon confirmation of recovery from the carrier or provider.
1 Healthline, 2 JAMA Networks, 3 Protenus, 4 Experian, 5 Bend HAS, 6 American Journal of Public Health


