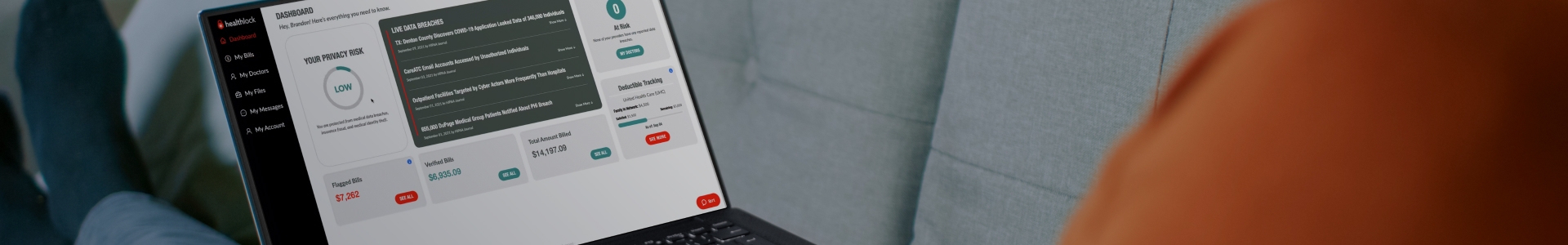
HealthLock Membership
HealthLock automatically reviews your medical claims and flags medical bill errors to help you save. Your membership covers your entire family, even if you have different insurance coverage.
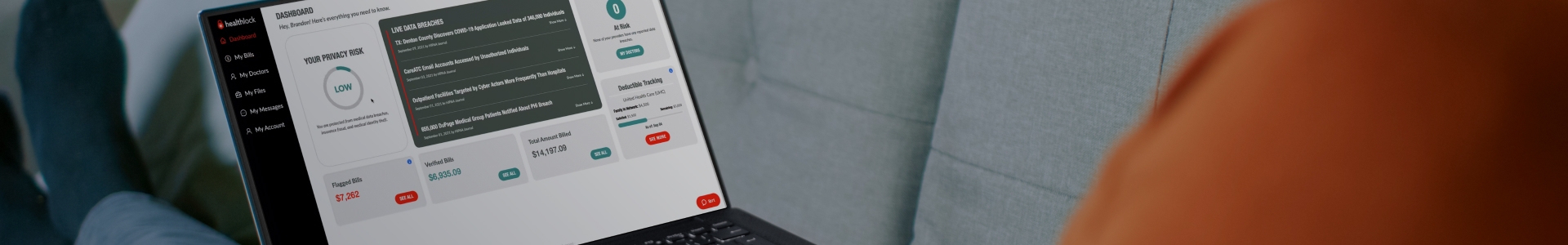
HealthLock automatically reviews your medical claims and flags medical bill errors to help you save. Your membership covers your entire family, even if you have different insurance coverage.